Mon Dec 29 2025
Why Nurses End Up Chasing Everyone During Discharge — And Why That's a System Failure
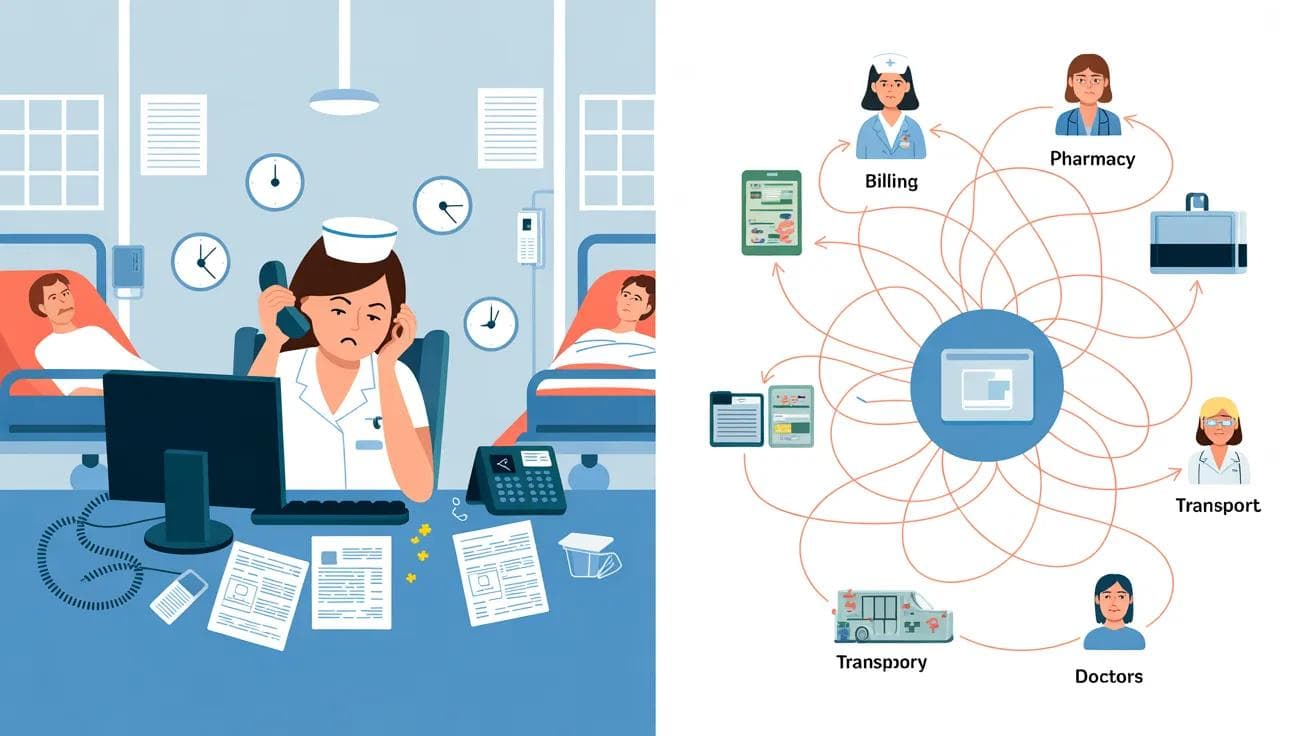
Discharge delays aren’t caused by unmotivated staff or missing software. They happen because coordination depends on nurses manually chasing billing, pharmacy, transport, and doctors. When ownership is fragmented and information doesn’t flow automatically, nurses become the system—leading to burnout, blocked beds, and frustrated families.
It’s 11:00 AM at a busy 150-bed hospital in Bangalore.
Nurse Priya receives a discharge order for Bed 304—a 62-year-old patient recovering from knee replacement surgery. Medically cleared. Ready to go home.
What should take 90 minutes will stretch until after 4 PM.
Here’s what the next five hours look like.
11:15 AM – Calls billing. No answer. Walks to the 3rd-floor billing office.
11:40 AM – Billing says TPA approval is pending. Calls insurance desk. On hold for 12 minutes.
12:00 PM – Walks to pharmacy (Building B). Discharge medications weren’t notified yet.
12:30 PM – Calls equipment room for a wheelchair. “We’ll send someone.” No one comes.
1:15 PM – Patient’s son calls the nurse station asking for an update. Priya doesn’t have one.
1:45 PM – Billing finally clears. She walks back to pharmacy to expedite medicines.
2:30 PM – Still no wheelchair. Priya walks to the basement equipment room herself.
3:15 PM – Discharge summary still unsigned. The resident doctor is in OT.
3:45 PM – Family arrives. Medications ready. Wheelchair ready. Waiting for the doctor.
4:10 PM – Patient finally leaves.
Total: 5 hours, 12 phone calls, and over 2 kilometers walked inside the hospital.
Priya returns to her station exhausted. She has six other patients who needed her attention today. She barely saw them.
This is not a Priya problem.
This is a system failure.
Why Nurses Become the Coordination Hub by Default
Ask a simple question inside most hospitals:
“Who owns the discharge?”
You’ll get different answers:
- “The doctor writes the order.”
- “Case management handles discharge.”
- “The ward nurse coordinates.”
- “It’s a team effort.”
When everyone is responsible, no one is accountable.
Here’s what actually happens:
- The doctor writes the discharge order and moves on.
- The case manager (if one exists) focuses on insurance, not logistics.
- Billing doesn’t know a discharge is planned until someone calls.
- Pharmacy waits for verbal confirmation because orders get cancelled.
- Equipment works first-come-first-served, with no urgency visibility.
- Families call the nurse station every 30 minutes asking, “Can we come?”
The only person seeing the full picture is the bedside nurse—because she is manually stitching it together.
So coordination collapses onto her.
Information Doesn’t Flow. It Has to Be Chased.
In a typical hospital, this is how discharge coordination really works:
- Doctor → Nurse: EMR order + verbal handoff
- Nurse → Billing: Phone call (often multiple attempts)
- Nurse → Pharmacy: Phone call or handwritten slip
- Nurse → Transport/Equipment: WhatsApp group message
- Nurse → Family: Repeated phone calls
Each handoff is manual.
Each delay needs follow-up.
Each follow-up pulls the nurse away from patient care.
Meanwhile:
- Billing doesn’t know the patient is medically cleared
- Pharmacy doesn’t know billing is waiting on TPA
- Transport doesn’t know medicines aren’t ready
- Family doesn’t know anything until they arrive
Everyone is working in isolation.
The nurse is the only integration layer.
Every Department Uses a Different System
Walk through the hospital and ask:
- Doctors: “We use the EMR.”
- Nurses: “EMR, WhatsApp, phone calls.”
- Billing: “Tally and a billing system.”
- Pharmacy: “Pharmacy software, mostly phone.”
- Transport/Equipment: “WhatsApp group and a register.”
- Families: “We call the nurse station.”
The nurse becomes the human API:
- Logging into systems she doesn’t own
- Calling departments she doesn’t control
- Tracking progress in her head or on paper
This isn’t coordination.
It’s heroic effort masking structural dysfunction.
The Hidden Costs of This Failure
For Nurses: Burnout from Coordination Overload
Studies in Indian hospitals show nurses spend 35–45% of their shift on coordination—not care.
That’s 3–4 hours per shift spent:
- Walking between departments
- Making follow-up calls
- Managing interruptions
- Handling frustration they didn’t create
Burnout rises. Engagement drops. Good nurses leave—not because of patients, but because of systems.
For Hospitals: Lost Revenue and Blocked Beds
For a 100-bed hospital:
- Average discharge time: 5–6 hours
- Optimal discharge time: ~90 minutes
- Time wasted per discharge: ~4 hours
If 30 beds turn over daily:
- 120 bed-hours lost per day
- Equivalent to 5 blocked beds
Annual impact:
- ~1,277 bed-days lost
- At ₹8,000 per bed-day → ₹1+ crore annually
And that excludes:
- Nurse overtime
- Delayed billing collections
- Reputation damage
For Patients and Families: Frustration and Risk
From the patient’s perspective:
- “You’re going home today” at 9 AM
- Still waiting at 3 PM
- Family loses a workday
- Anxiety builds
- Infection risk increases
Clinical care may be excellent—but the experience feels chaotic.
Why Common Fixes Don’t Work
“Hire more discharge coordinators”
Adds cost, not flow. Still manual. Still blind.
“Use the EMR for coordination”
EMRs are systems of record, not systems of action:
- Desktop-first
- Limited access
- No real-time nudging or escalation
“Create WhatsApp groups”
Unstructured chat creates noise, not accountability.
Messages get lost. Ownership is unclear. Nothing closes cleanly.
WhatsApp groups create the illusion of coordination.
What a System-Level Solution Looks Like
A real solution does three things:
1. Information Moves Automatically
Discharge order → instant notifications to billing, pharmacy, equipment, family—without nurse chasing.
2. People Use Tools They Already Have
No new apps. No training. WhatsApp becomes the action surface, not the memory.
3. Accountability Is Built In
Clear owners. SLAs. Auto-escalation. Shared visibility.
The nurse monitors progress instead of driving it.
The Shift Hospitals Must Make
The question isn’t:
“Why are nurses always chasing?”
It’s:
“Why does our system require them to?”
Until coordination is owned by the system, nurses will keep compensating—quietly, exhaustingly, and unsustainably.
Fix the system, and nurses go back to what they’re trained for: caring for patients.
Written by
Prasanna K Ram
CEO
View LinkedIn Profile